Medicare controls the fees it pays. What it pays as a percentage of what is billed varies by many factors, but in many cases it is a very small portion. Here is a real life example of the expenses associated with a cataract operation.

The amounts shown left to right are Billed, Allowed and Paid by Medicare. The fees are the ophthalmologist, anesthetist and outpatient surgical center top to bottom.
All this information is shown to the Medicare beneficiary, in other words transparent. So what’s the problem? Do you think those allowed fees are too high? I think $8,000 as billed is outrageous, but I don’t think $2,000 as allowed is.
The problem is (over) utilization and that problem is something that can only be managed by the plan administrator; (in this case CMS)… which is exactly what the CBO assumed will be done by private plans when it lowered it cost estimate for Obamacare.
Given how Medicare works and determines what it will pay, you have to wonder why the physicians billed charge is shown at all or is even relevant. Why don’t physicians simply indicate the procedure code and be done with it?
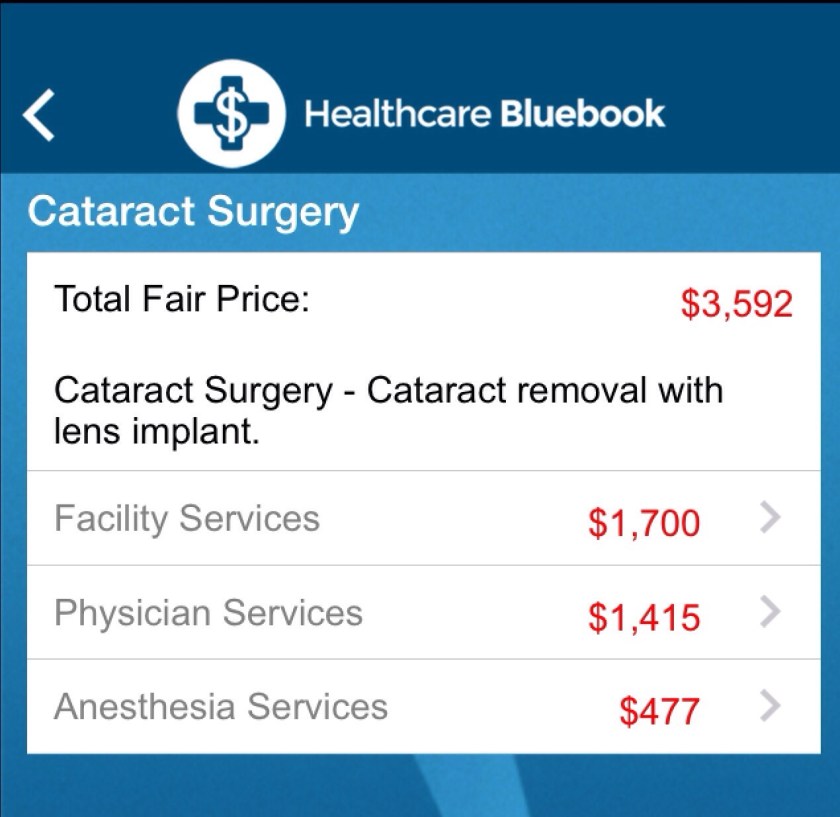
You also have to wonder how our system really works when for these same services the providers will be paid differently by Medicare, Medicaid, and each insurance plan whether they participate or not. Exactly what is the fair price? Nobody knows.
Here is an example from the Healthcare Bluebook which reflects the charges physicians typically accept from private insurance companies. The first set of fees is from North Jersey and the second from Minneapolis. Note how they compare with Medicare for the same services.

Even if we assume that a truly fair price is between these private sector and Medicare allowable fees, it is clear that the private sector is subsiding Medicare. If on the other hand the Medicare fee is fair and adequate, then you know why health care in America is so expensive.


One comment